Did you think homeopathy was not publicly funded in Australia? It is.
There has been lots of talk recently in the Australian media about CAM in universities. A new lobby group known as Friend of Science in Medicine was recently established to get the discussion going about whether this is a good thing. (Full disclosure, I recently added my name to the 400-long list of doctors, scientists and concerned citizens who are worried about pseudoscience creeping into universities).
The discussion has ruffled some feathers and I think this is a good thing. As I said in a comment on The Conversation, what is wrong with us looking at these courses and determining if what they are teaching is evidence-based? If we find there is nothing wrong, then we can carry on our merry way.
Yet, some CAM peeps don’t seem to see it this way. Some have been behaving as if they are being persecuted. Some are claiming that taking CAM out of unis puts the public at risk as practitioners are more likely exposed to shonky teaching (I haven’t seen any evidence for this, but as usual I’m willing to look at it if it’s true).
But this misses the point that it doesn’t matter where you teach it, if it’s nonsense outside of a university it remains nonsense when taught in one. Teaching homoeopathy or tactile therapy in a university environment won’t make it work. To see how homeopathy works, go here.
The argument got rather heated on Twitter recently with Prof Kerryn Phelps jumping in the mix. I had quite a long conversation with her, which remained mostly civil (if not a little strained) until I suggested we weed out the stuff we know doesn’t work or exist, such as subluxations in chiropractic and homeopathy.
The response I got was odd to say the least and I’m still unsure exactly what she was getting at. See the screen shot below (read from bottom up).
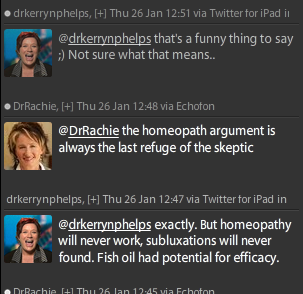
Some people suggested this was an example of the No True Scotsman fallacy, which I kinda agree with. More simply, it appears to say “don’t mention homoeopathy, even we’re embarrassed by that”. If you have another idea, please leave a comment.
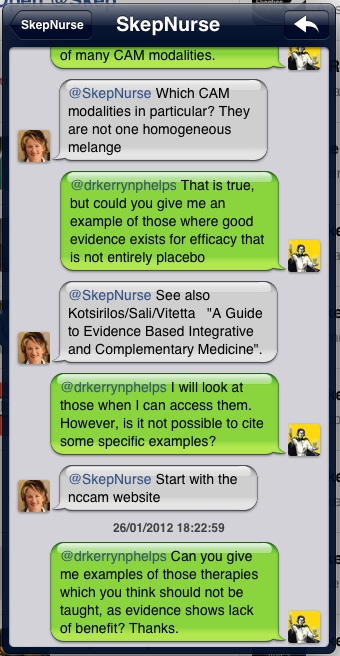
Someone else called “SkepNurse” also posed the question to Prof Phelps regarding which CAM she would unequivocally say was not worth pursuing any more, either because it can never work or has been proven not to. She posted these tweets on Jan 26th and is still awaiting a direct answer.
Anyway, I’d been poking around for information on whether homeopathy was taught in universities as a stand alone course, and I hadn’t found any evidence. CAM practitioners had confirmed this as well, pointing out that it was a requirement to enter Bachelor of Health Science (Complementary Medicine) at Charles Sturt University but was not taught as a separate subject.
Well, they were wrong.
Homeopathy is taught as a stand alone course subject at a publicly funded university in NSW as part of Southern Cross University’s Bachelor of Clinical Sciences. They offer introductory homeopathy and clinical homeopathy. It is also offered as a service in the health clinic
There is even a prize offered at SCU.
The Warren Brauer Memorial Prize – Homoeopath Dispensary to the value of $500
Awarded to the Naturopathy award graduate who has exhibited a high level of proficiency in the understanding and application of homeopathy.
Donated by Brauer Natural Medicine Pty Ltd
SCU is a publicly funded university who received $32 million of federal funding in 2011. Thus, public funding is going towards the teaching of nonsense in Australian Universities.
When I’ve previously written about public funding for homeopathy in Australia the most I could do was speculate about how much it might cost the tax payer. It’s complicated because our public health system does not directly fund homeopathy as health care, but it does supplement private health funds (which do cover homoeopathy) and also some doctors/gps will prescribe recommend it.
This is the first evidence I have found that tax payers funds directly fund this nonsense. And what a waste of money it is.
I’ve written to SCU to ask for their course outlines for both classes. Let’s hope I get them so I can get a better idea of exactly what they teach.
With continued pressure from FSM, this conversation will likely continue for some time. I would like to see the first casualty be these courses at SCU.
This comment on The Conversation has really summed up this debate for me so far. It’s from Didier Nave, an ex-herbalist of 25 years and the following excerpt speaks volumes;
Time to face the facts. The data is coming in and its not looking good. It’s clearly showing that what we do is not much better than placebo. So the question is do we have the humility to accept the evidence and dump these theories. I doubt it….Have i seen the industry contest or reject its own stupidities like live blood analysis or “detoxing” when it can’t name one toxin that its methods supposedly detox? No, it embraces them instead.”
=====
To see how The Dean of the School of Health, Professor Iain Graham, defends woo in his uni, see Mick Vagg’s post here.
There’s more info on woo in public and non-public facilities here.
Thanks to Loretta Marron for assisting with research.
—
More interesting reading on the current debate (and for healthy discussion in comments) see two recent articles from The Conversation;
Alternative Medicine Can Be Sientific Say Besieged Academics
Pointing The Bone At Chiropractic Quackery Lessons From the UK
—
To see the investigation of woo in universities from The Skeptic magazine (and written by Tim Mendham with research from Jo Benhamu) go here (pdf).